Part-C 2019 Cut Points
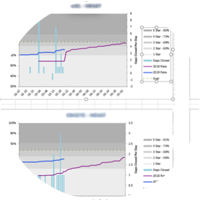
The graphs below display the 2018 to 2019 percent change of cut-points for each measure in Part-C, displaying a separate graph for each Star Rating. The red bars pictured represent data for measures increasing in difficulty, i.e. higher thresholds; while green bars will represent data related to lower thresholds. Numerous factors may alter a measure’s outcome for a health plan. Therefore, it is important to analyze these changes for opportunities to improve measure scores and overall performance.
2 Stars
The most noticeable change for the 2-star cut-points occurred with C09 – Care for Older Adults Medication Review. During 2018, the cut-point was set at 59% to reach 2 stars, but for 2019 that same score would garner only 1 star. This created a huge outlier in the data set because it represented the largest change of all the 2-star values for Part-C. Another notable cut-point change was seen with C10 – Care for Older Adults Functional Status Assessment with -70% decrease in difficulty. Lastly, C21 – Plan All Cause Readmissions and C30 – Members Choosing to Leave the Plan both decreased in difficulty by 50%. The major increase in difficulty for 2 stars cut points occurred with C20 – Medication Reconciliation Post Discharge with a 48% increase.
3 stars
For the 3 Stars cut-point C09 – Care for Older Adults-Functional Status Assessments and C-29 Complaints About Health Plan showed a 46% and 70% decrease in difficulty. Again, we see C20 – Medication Reconciliation Post Discharge with a 31% increase in difficulty. In addition, C30 - Members Choosing to Leave Health Plan and C34 - Call Center Foreign Language Interpreter and TTY Availability both increased by 25%.
4 stars
As for thresholds related to 4 stars, the major changes occurred with C29 – Complaints About the Health Plan with a 72% decrease in difficulty. To a lesser extent we see 18% decrease in difficulty in C30 – Members Choosing to Leave the Health Plan.
5 Star
Finally, there is our review of thresholds for Part-C measures for the coveted 5 stars. C029 - Complaints about the Health Plan had the largest jump amongst all measures. C029 decreased in difficulty by 40% making this measure potentially more obtainable. Following close behind this metric with decreasing difficulty is C30 - Members Choosing to Leave the Plan and C31 - Health Plan Quality Improvement. C30 decreased in difficulty by 33% and C31 by 28%. Alternatively, C21 – Plan All- Cause Readmissions received a 20% increase in difficulty meaning health plans may have to put in extra effort to reach 5 stars for this measure.
The Centers for Medicare & Medicaid Services (CMS) is a federal agency within the United States Department of Health and Human Services (HHS) that administers the Medicare program and works in partnership with state governments to administer Medicaid in addition to other programming. CMS releases guidance throughout the year to keep health plan, providers, and practitioners in the know as to the management of the Stars program. At Baltimore Health Analytics, our mission is to meet you where you are, fill your need gaps, and pivot to wherever the opportunity is using our specialized clinical strategy, software design, and analytic skills. Our philosophy is that you should always be looking for your next "best move" while always being ready for the next opportunity. baltimorehealthanalytics.com.